April 2022
Understanding the Risks of PAD
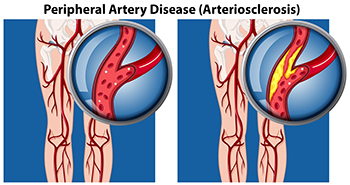
PAD or Peripheral Artery Disease occurs when there is a narrowing or blockage of blood vessels. This disease is caused by a buildup of fat in the arteries, and is also known as atherosclerosis. Though this can happen in any blood vessel, it is more common in the lower extremities. Risks for PAD include aging, smoking, high blood pressure, high cholesterol, and diabetes. Some symptoms that may be present include pain in the feet or legs with activity that stops with rest, decreased or absent foot pulse, sores or ulcers that do not heal, and cold or numb toes. Beyond damage to one’s feet if left untreated, PAD can lead to a heart attack or stroke. If you have any of these symptoms, it is important to see a podiatrist to measure blood pressure in the ankles via an ankle brachial index (ABI) and compare that to blood pressure in the arms, do possible imaging studies, confirm the diagnosis, and obtain a treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Where Heel Pain Occurs May Provide Clues to Its Cause

Heel pain can be caused by a variety of conditions, with the most common one being plantar fasciitis: an inflammation of the plantar fasciitis tissue on the bottom of the foot. Identifying where the pain is specifically located in the heel can sometimes help your podiatrist diagnose your condition. For instance, plantar fasciitis usually causes pain in the bottom/middle of the heel which is at its worst when you first wake up in the morning. Other conditions, such as heel stress fractures, nerve issues, or heel pad atrophy can also cause pain on the bottom of the heel. Pain in the back of the heel may be caused by problems with your Achilles tendon, which connects the heel bone to the calf muscles. These conditions include Achilles tendinopathy/tendinitis, which is usually an overuse injury to the tendon, Haglund’s deformity, which produces a bump at the back of the heel due to shoes exerting pressure on the tendon, and Sever’s disease, which is due to stress on the heel’s growth plate in growing children. Pain in the middle of the heel can sometimes be caused by an entrapped nerve in the ankle (tarsal tunnel syndrome). Sinus tarsi syndrome, typically due to flat feet or following an ankle sprain, can cause pain in the middle/side portion of the heel. Any type of heel pain should be examined by a podiatrist to receive proper diagnosis and treatment.
Many people suffer from bouts of heel pain. For more information, contact Dr. Mark Spier of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Medical Issues May Lead to Poor Circulation
 Poor circulation in the feet may be indicative of serious medical issues in the body. It happens when there isn't enough blood being carried to the feet, and generally develops from blocked arteries. Additional reasons may include smoking, an unhealthy diet, or sitting and standing for extended periods of time. Common symptoms many patients notice include cold feet, a numbing or tingling sensation, pain while walking. Noticeable signs of poor circulation can consist of dry skin, swollen feet, and the toes may look discolored. Mild relief may be found when a gentle exercise program is practiced, elevating the legs as often as possible, and it can help to wear compression stockings. If you have any of these symptoms, it is advised that you schedule an appointment with a podiatrist who can help you to manage poor circulation.
Poor circulation in the feet may be indicative of serious medical issues in the body. It happens when there isn't enough blood being carried to the feet, and generally develops from blocked arteries. Additional reasons may include smoking, an unhealthy diet, or sitting and standing for extended periods of time. Common symptoms many patients notice include cold feet, a numbing or tingling sensation, pain while walking. Noticeable signs of poor circulation can consist of dry skin, swollen feet, and the toes may look discolored. Mild relief may be found when a gentle exercise program is practiced, elevating the legs as often as possible, and it can help to wear compression stockings. If you have any of these symptoms, it is advised that you schedule an appointment with a podiatrist who can help you to manage poor circulation.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Dr. Mark Spier of Maryland. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are Bunions Affecting Your Everyday Life?
What Does Plantar Fasciitis Feel Like?
If you have pain that is located anywhere on the sole of your foot—throughout the heel or in the arch—you may be suffering from plantar fasciitis. The discomfort associated with plantar fasciitis may be an aching or dull pain, or even a burning or sharp pain. Plantar fasciitis pain is typically at its most severe when you first wake up in the morning, or after periods of rest. What causes plantar fasciitis pain? It occurs when the plantar fascia tissue that spans the bottom of the feet and connects the toes with the heel becomes inflamed due to tiny micro tears. Plantar fasciitis is usually the result of repetitive overuse, however, there are other possible causes and a variety of contributing factors. A podiatrist can help pinpoint why you developed this condition, treat it accordingly, and help prevent it from returning.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Mark Spier from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.











