How Your Arch Is Formed and Why It Might Be Painful

The arch of the foot is critical in dispersing body weight throughout the foot. It also helps a person balance and propel themselves forward when they walk. This important structure made of tendons, bones and ligaments is a combination of three separate arches forming a triangular shape. The transverse arch spans the ball of the foot from side-to-side. The two other arches run from the ball of the foot to the heel: the lateral arch on the outside and the medial arch on the inside of the foot. If you feel pain in your arch it may be due to an inflammation of the plantar fascia tissue which supports the arch (plantar fasciitis). Or, you may have flat feet, which can cause your feet to roll excessively inward when you walk (overpronation) and flatten your arches. An abnormally high arch can also stress your ankle and cause pain. Even an inflammation of the posterior tibial tendon, which connects the inner area of the foot to a calf muscle, can cause pain in the arches. If your arches are painful, it's wise to call a podiatrist who will be able to properly diagnose and treat the area and discuss treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
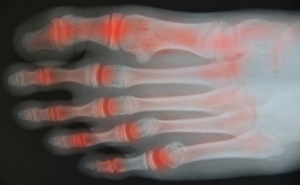
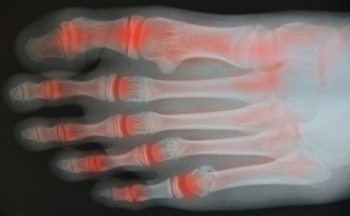
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Big Toe Arthritis Relief
Arthritis in the first metatarsal phalangeal (MTP) or big toe joint is common, particularly as one begins to age. We use our feet to get us through life and normal walking, other movements, and wearing high heeled or improperly fitting shoes can stress the main joint of the big toe. Osteoarthritis or Hallux Rigidus is the most common arthritic condition affecting this joint and it can be quite painful and limit movement. The big toe may also become stiff and swollen. The best treatment for this condition is a fusion of the joint. The procedure fuses or welds together the two bones that make up the aching joint. It does not make the toe less stiff or restore motion, but it relieves the pain. An alternative procedure is a joint replacement of the big toe, but it is not ideal because the use of metal and plastic has not been successful in this type of joint replacement. It is not predictable in relieving pain, and repeated force on the joint with each step makes it less long-lasting than bigger joints, like the knee and hip. Options for treatment of a failed replacement are limited and may be replaced with bone grafting and joint fusion. If you suffer from pain in the joints of the big toe, consult with a podiatrist for the best treatment plan for you.
In certain cases, in which the patient suffers from extreme pain or damage in a joint, joint replacement surgery may be deemed useful. If you have constant pain in a foot joint, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Joint Replacement Surgery?
Over time, joints wear down; this can be exacerbated by diseases and conditions. Joint replacement surgery, also known as arthroplasty, is when a damaged joint is surgically removed and replaced with a prosthesis. Prostheses, which can be made of ceramic, plastic, or metal, act as joints in lieu of an actual joint. One of the most prevalent causes for joint replacement is arthritis.
Arthritis in the Foot
Arthritis can occur in any joint in the body, including in the feet. Common types of arthritis in the foot are osteoarthritis, rheumatoid arthritis, and gout. The big toe is usually where arthritis occurs in the foot; this is known as hallux rigidus.
Joint Replacement Surgery in the Foot
The most common form of joint replacement in the foot is a first metatarsophalangeal (MTP) joint placement. MTP joint replacement surgery is designed to treat hallux rigidus. Surgery is not intensive, and recovery occurs within one to two months after the procedure has been done. Overall, joint replacement surgery is a safe and effective way to treat pain in the joint of the foot.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Joint Replacement Surgery
When conservative, noninvasive treatments prove unsuccessful, podiatrists will often turn to surgery as the last line of treatment for their patients. If patients are suffering from joint pain, issues in mobility, or are seeking to correct a deformity, joint replacement surgery is an effective option. Joint replacement surgery is also successful in treating arthritis, which is the most common cause of improperly working joints.
Patients with symptoms that include joint pain, stiffness, limping, muscle weakness, limited motion, and swelling are typically considered for joint replacement surgery. Range of motion and activity post-surgery will vary between patients and depending on the specific surgery performed, the affected joint, and the damage that will need to be repaired.
Joint replacement surgery replaces the damaged cartilage and bone, the latter if required. The damaged cartilage is typically replaced with a prosthesis that is attached to the bone, allowing the implant to grow into the bone. Following surgery, the patient will typically undergo physical therapy to become familiar with movement using the replaced joint.
Understanding the Risks of PAD
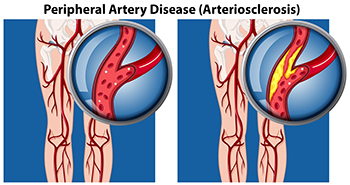
PAD or Peripheral Artery Disease occurs when there is a narrowing or blockage of blood vessels. This disease is caused by a buildup of fat in the arteries, and is also known as atherosclerosis. Though this can happen in any blood vessel, it is more common in the lower extremities. Risks for PAD include aging, smoking, high blood pressure, high cholesterol, and diabetes. Some symptoms that may be present include pain in the feet or legs with activity that stops with rest, decreased or absent foot pulse, sores or ulcers that do not heal, and cold or numb toes. Beyond damage to one’s feet if left untreated, PAD can lead to a heart attack or stroke. If you have any of these symptoms, it is important to see a podiatrist to measure blood pressure in the ankles via an ankle brachial index (ABI) and compare that to blood pressure in the arms, do possible imaging studies, confirm the diagnosis, and obtain a treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Where Heel Pain Occurs May Provide Clues to Its Cause

Heel pain can be caused by a variety of conditions, with the most common one being plantar fasciitis: an inflammation of the plantar fasciitis tissue on the bottom of the foot. Identifying where the pain is specifically located in the heel can sometimes help your podiatrist diagnose your condition. For instance, plantar fasciitis usually causes pain in the bottom/middle of the heel which is at its worst when you first wake up in the morning. Other conditions, such as heel stress fractures, nerve issues, or heel pad atrophy can also cause pain on the bottom of the heel. Pain in the back of the heel may be caused by problems with your Achilles tendon, which connects the heel bone to the calf muscles. These conditions include Achilles tendinopathy/tendinitis, which is usually an overuse injury to the tendon, Haglund’s deformity, which produces a bump at the back of the heel due to shoes exerting pressure on the tendon, and Sever’s disease, which is due to stress on the heel’s growth plate in growing children. Pain in the middle of the heel can sometimes be caused by an entrapped nerve in the ankle (tarsal tunnel syndrome). Sinus tarsi syndrome, typically due to flat feet or following an ankle sprain, can cause pain in the middle/side portion of the heel. Any type of heel pain should be examined by a podiatrist to receive proper diagnosis and treatment.
Many people suffer from bouts of heel pain. For more information, contact Dr. Mark Spier of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.