Pain in the Ball of the Foot

Pain in the ball of the foot can be a discomforting and debilitating issue that can affect daily activities. This type of pain can occur due to various factors, including excessive pressure, overuse, or structural abnormalities in the foot. Metatarsalgia, a condition characterized by inflammation and pain in the ball of the foot, is a common culprit. High-impact activities, prolonged standing, and wearing improper footwear with inadequate support can exacerbate the pain. Additionally, conditions such as Morton's neuroma, sesamoiditis, and arthritis can contribute to discomfort in this area. Individuals may experience symptoms like burning, tingling, or numbness in the ball of the foot, making it challenging to walk or stand for extended periods. Proper footwear selection, orthotics, and rest are essential for alleviating pain and preventing further injury. If you have pain in the ball of your foot, it is suggested to seek treatment from a podiatrist who can help identify the underlying cause and develop an effective management plan.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Nutritional Needs for Diabetic Foot Ulcer Recovery

Addressing the nutritional needs of individuals with diabetic foot ulcers is a critical part of promoting healing and preventing more serious problems. Stable blood sugar levels, achieved through monitoring carbohydrate intake on a regular basis, are vital for managing diabetes and promoting optimal healing of foot ulcers. A well-balanced diet is also essential in supporting the body's natural wound healing processes. Protein-rich foods like poultry, fish, eggs, and legumes aid in tissue repair and wound healing. Additionally, vitamins and minerals such as vitamin C, zinc, and vitamin E enhance immune function and collagen synthesis, facilitating wound healing. Fruits, vegetables, whole grains, and healthy fats provide antioxidants and anti-inflammatory compounds to support overall health and reduce infection risk. If you have diabetes and have developed a foot ulcer, it is suggested that you consult a podiatrist to discuss optimal healing methods, including important nutritional needs, tailored to your specific condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Mark Spier from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
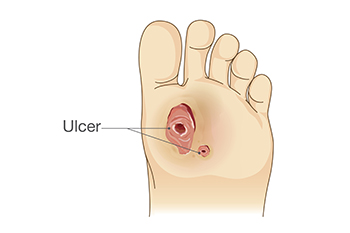
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Early Diagnosis and Treatment of Rheumatoid Arthritis

Rheumatoid arthritis, also known as RA, is a prevalent inflammatory condition, affecting up to one percent of the global population. It can develop at any age but is most common in individuals that are between 30 and 50 years old, with significant disability implications. Genetic factors play a substantial role, with approximately half the risk attributable to genetic predisposition, including specific human leukocyte antigen associations. Smoking is a major environmental trigger. RA primarily affects joints, leading to synovial inflammation, cartilage damage, and bone erosion. Symptoms include joint pain, stiffness, and swelling, often affecting the toes of the feet. Morning stiffness lasting over an hour is a hallmark sign. If you have discomfort in your feet from RA, it is suggested that you schedule an appointment with a podiatrist, as prompt diagnosis is essential for early intervention and management to mitigate joint damage and preserve joint function.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Mark Spier of Maryland. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
Understanding Slow Wound Healing in Diabetic Patients
Wound healing is a complex process that can be significantly delayed in diabetic patients due to various physiological factors. High blood sugar levels characteristic of diabetes can impair the body's ability to repair damaged tissue by disrupting the function of immune cells, such as macrophages and neutrophils, responsible for combating infections and initiating the healing process. Additionally, diabetes often leads to poor circulation, reducing the delivery of oxygen and nutrients to the site of the wound, which is essential for tissue regeneration. Peripheral neuropathy, another common complication of diabetes, causes nerve damage and diminishes sensation in the extremities, making it difficult for patients to detect injuries and ulcers in their early stages. Furthermore, compromised immune function and increased susceptibility to infections further hinder the healing process. Managing blood sugar levels, maintaining proper foot care, and seeking prompt medical attention for wounds are crucial steps in minimizing the risk of complications and promoting effective wound healing in diabetic individuals. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can provide you with effective wound prevention tips, in addition to helping you manage this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Bursitis as a Cause of Heel Pain
 Bursa, an important cushion between your muscles and bone, can sometimes cause heel pain if it becomes inflamed or irritated. This condition, called bursitis, often occurs due to repetitive stress on the ankle from running, jumping, and walking. Bursitis in the heel can make activities like walking or standing for long periods painful. Your heel may also be red and tender to the touch. You may be at an increased risk for this condition if you have a history of inflammatory arthritis or suddenly start intense workout routines. The good news is that with proper care and attention, individuals with heel pain from bursitis can find relief and improve their overall foot health. If you are experiencing persistent heel pain, it is suggested that you consult a podiatrist who can diagnose the source of the pain, and provide personalized treatment.
Bursa, an important cushion between your muscles and bone, can sometimes cause heel pain if it becomes inflamed or irritated. This condition, called bursitis, often occurs due to repetitive stress on the ankle from running, jumping, and walking. Bursitis in the heel can make activities like walking or standing for long periods painful. Your heel may also be red and tender to the touch. You may be at an increased risk for this condition if you have a history of inflammatory arthritis or suddenly start intense workout routines. The good news is that with proper care and attention, individuals with heel pain from bursitis can find relief and improve their overall foot health. If you are experiencing persistent heel pain, it is suggested that you consult a podiatrist who can diagnose the source of the pain, and provide personalized treatment.
Many people suffer from bouts of heel pain. For more information, contact Dr. Mark Spier of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.