March 2022
Why Do I Get Blisters on My Feet?
Blisters are usually caused by friction of something rubbing against the skin. A red, painful, swollen sore can develop on the foot from constant rubbing of a shoe, sock or other rough surface against the skin. This often turns into a blister. Interestingly, a blister is the body’s way of forming a protective shield filled with liquid to protect more delicate underlying tissue. Blisters can also be caused by less obvious irritants, burns, frostbite, or underlying health conditions. In many cases, one can just leave the blister alone and it will heal with basic care. It is important not to puncture the blister. If a blister gets worse, does not heal, or becomes discolored, it is suggested that you see a qualified podiatrist for proper diagnosis and treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Mark Spier of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
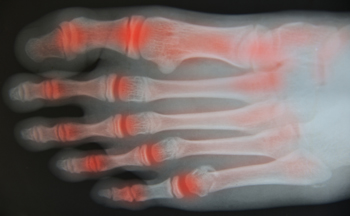
When Rheumatoid Arthritis Affects the Ankle
Rheumatoid arthritis (RA) is a progressive disease that causes the body’s immune system to mistakenly attack healthy tissue. RA can break down cartilage between bones in the ankle. Without healthy cartilage between ankle bones, bones rub together and cause friction that can lead to inflammation and pain in the ankle joint. In addition, RA can also weaken surrounding tissues that normally support and stabilize the ankle. Over time, the damage RA inflicts on the ankle can change how the joint functions and may lead to further destruction. A podiatrist can diagnose RA in your ankles and help determine the best course of treatment, which may include non-steroidal anti-inflammatory medications, corticosteroid injections, custom orthotics, physical therapy, and in some cases, surgery.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Mark Spier from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Types of Athlete's Foot
 The most common type of athlete’s foot is referred to as chronic interdigital. Symptoms that are associated with this condition often include itchiness between the toes and on the bottom of the foot. It can develop as a result of wearing shoes that are too small, and this can create a warm environment that is perfect for fungus to grow in. The least common type of athlete’s foot is known as vesicular, and this can produce blisters that are painful on the bottom or top of the foot. Athlete’s foot is contagious and may be prevented by wearing appropriate shoes in public showers. If you have developed this uncomfortable foot condition, it is strongly suggested that you consult with a podiatrist who can begin the correct treatment for you.
The most common type of athlete’s foot is referred to as chronic interdigital. Symptoms that are associated with this condition often include itchiness between the toes and on the bottom of the foot. It can develop as a result of wearing shoes that are too small, and this can create a warm environment that is perfect for fungus to grow in. The least common type of athlete’s foot is known as vesicular, and this can produce blisters that are painful on the bottom or top of the foot. Athlete’s foot is contagious and may be prevented by wearing appropriate shoes in public showers. If you have developed this uncomfortable foot condition, it is strongly suggested that you consult with a podiatrist who can begin the correct treatment for you.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. Mark Spier from Maryland. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are You Suffering From Ingrown Toenails?
What Is a Walking Boot?
A walking boot is an orthotic device used to protect the foot or ankle after an injury. The boot helps keep the foot stable and in the right position so that it can heal properly. Walking boots can also help keep weight and pressure off of an injured area. Injuries that may require wearing a walking boot include broken bones, tendon injuries, severe sprains, and shin splints. Most walking boots have two to five adjustable straps that hold the boot in place over the injured leg. How long you will need to wear the walking boot will depend on your specific injury and its severity. For more information, please consult with a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Mark Spier from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
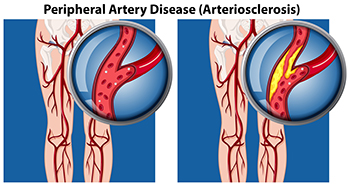
How to Care For Your Feet if You Have PAD
Peripheral arterial disease (PAD) is a circulatory condition that reduces blood flow to the limbs. It can lead to leg pain and cramping when walking, coldness in the feet and lower legs, no or weak pulse in the legs, non-healing sores, and more. If you have PAD, you are more at risk of developing ulcers and infections, so it is important to take good care of your feet with the following tips. Keep your feet clean, dry, and moisturized. Your toenails should be trimmed straight across, but not so short that the nail grows into the surrounding skin and causes an ingrown toenail. Keep your feet protected from extreme heat or cold, always wear shoes and socks, and never go barefoot. You should inspect your feet entirely every day. Look for any cuts, bruises, bumps, swelling or red spots in the skin that may develop into a wound. Because of your condition, you should seek the care of a podiatrist if you detect any cuts or possible infections in order to receive proper treatment, and to avoid making the situation worse.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.