February 2024
Nutritional Needs for Diabetic Foot Ulcer Recovery

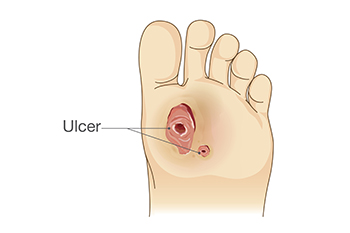
Addressing the nutritional needs of individuals with diabetic foot ulcers is a critical part of promoting healing and preventing more serious problems. Stable blood sugar levels, achieved through monitoring carbohydrate intake on a regular basis, are vital for managing diabetes and promoting optimal healing of foot ulcers. A well-balanced diet is also essential in supporting the body's natural wound healing processes. Protein-rich foods like poultry, fish, eggs, and legumes aid in tissue repair and wound healing. Additionally, vitamins and minerals such as vitamin C, zinc, and vitamin E enhance immune function and collagen synthesis, facilitating wound healing. Fruits, vegetables, whole grains, and healthy fats provide antioxidants and anti-inflammatory compounds to support overall health and reduce infection risk. If you have diabetes and have developed a foot ulcer, it is suggested that you consult a podiatrist to discuss optimal healing methods, including important nutritional needs, tailored to your specific condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Mark Spier from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Early Diagnosis and Treatment of Rheumatoid Arthritis

Rheumatoid arthritis, also known as RA, is a prevalent inflammatory condition, affecting up to one percent of the global population. It can develop at any age but is most common in individuals that are between 30 and 50 years old, with significant disability implications. Genetic factors play a substantial role, with approximately half the risk attributable to genetic predisposition, including specific human leukocyte antigen associations. Smoking is a major environmental trigger. RA primarily affects joints, leading to synovial inflammation, cartilage damage, and bone erosion. Symptoms include joint pain, stiffness, and swelling, often affecting the toes of the feet. Morning stiffness lasting over an hour is a hallmark sign. If you have discomfort in your feet from RA, it is suggested that you schedule an appointment with a podiatrist, as prompt diagnosis is essential for early intervention and management to mitigate joint damage and preserve joint function.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Mark Spier of Maryland. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Slow Wound Healing in Diabetic Patients
Wound healing is a complex process that can be significantly delayed in diabetic patients due to various physiological factors. High blood sugar levels characteristic of diabetes can impair the body's ability to repair damaged tissue by disrupting the function of immune cells, such as macrophages and neutrophils, responsible for combating infections and initiating the healing process. Additionally, diabetes often leads to poor circulation, reducing the delivery of oxygen and nutrients to the site of the wound, which is essential for tissue regeneration. Peripheral neuropathy, another common complication of diabetes, causes nerve damage and diminishes sensation in the extremities, making it difficult for patients to detect injuries and ulcers in their early stages. Furthermore, compromised immune function and increased susceptibility to infections further hinder the healing process. Managing blood sugar levels, maintaining proper foot care, and seeking prompt medical attention for wounds are crucial steps in minimizing the risk of complications and promoting effective wound healing in diabetic individuals. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can provide you with effective wound prevention tips, in addition to helping you manage this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Mark Spier from Maryland. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bursitis as a Cause of Heel Pain
 Bursa, an important cushion between your muscles and bone, can sometimes cause heel pain if it becomes inflamed or irritated. This condition, called bursitis, often occurs due to repetitive stress on the ankle from running, jumping, and walking. Bursitis in the heel can make activities like walking or standing for long periods painful. Your heel may also be red and tender to the touch. You may be at an increased risk for this condition if you have a history of inflammatory arthritis or suddenly start intense workout routines. The good news is that with proper care and attention, individuals with heel pain from bursitis can find relief and improve their overall foot health. If you are experiencing persistent heel pain, it is suggested that you consult a podiatrist who can diagnose the source of the pain, and provide personalized treatment.
Bursa, an important cushion between your muscles and bone, can sometimes cause heel pain if it becomes inflamed or irritated. This condition, called bursitis, often occurs due to repetitive stress on the ankle from running, jumping, and walking. Bursitis in the heel can make activities like walking or standing for long periods painful. Your heel may also be red and tender to the touch. You may be at an increased risk for this condition if you have a history of inflammatory arthritis or suddenly start intense workout routines. The good news is that with proper care and attention, individuals with heel pain from bursitis can find relief and improve their overall foot health. If you are experiencing persistent heel pain, it is suggested that you consult a podiatrist who can diagnose the source of the pain, and provide personalized treatment.
Many people suffer from bouts of heel pain. For more information, contact Dr. Mark Spier of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Columbia and Reisterstown, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.









